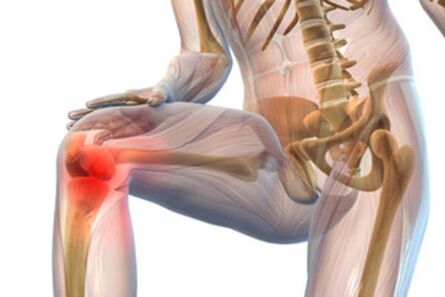
Arthrosis (gonarthrosis) of the knee joint is a degenerative change in the joint that eventually leads to deformity. In this, cartilage tissue begins to collapse. The function of the knee gradually deteriorates and the patient loses the ability to move normally. This disease is very common.
Treating arthrosis of the knee joint is long-term, but it cannot completely cure the problem. However, therapy is needed to maintain joint mobility and functionality for as long as possible and to improve the patient’s quality of life.
Types of diseases
It is possible to classify gonarthrosis of the knee joint due to the causes of its development. Primary and secondary. The first type of disease is the most common. It also has another name - idiopathic osteoarthritis. The exact cause of this form of knee osteoarthritis is difficult to determine because there are too many influencing factors.
The secondary type of pathology is clearly related to one cause or another. For example, it often occurs after a knee injury due to severe physical exertion of the knee joint. Such gonarthrosis is often genetically determined. Certain diseases can also cause dystrophic changes in the knee joint: diabetes mellitus, rheumatoid arthritis, congenital deformity of the lower extremities.
Why pathology develops
The knee joint is one of the most complex joints in the human body. It is made up of the femur, tibia and patella. Articulation also includes curved-edged triangular cartilage - meniscus. The well-coordinated work of the knee is ensured by the muscle-tape device. Almost all bone surfaces of the joint are covered with cartilage tissue with a thickness of approx. 0, 5 cm. It feeds on blood vessels as well as in a diffuse way (it obtains useful substances from the synovial fluid).
The cartilage of the knee allows the bony surfaces to slip and cushion. When the nutrition of this tissue is disturbed, dystrophic processes begin in it, it becomes thinner. Without treatment, the cartilage disappears completely and the knee joint stops. The cause of arthrosis can be different. For example, the following factors may provoke the appearance of a secondary form of pathology:
- Excessive stress on the knee joint. In this case, changes may occur that the person is not aware of. Therefore, the load should be moderate, especially in old age. The biggest damage is squatting and running on hard surfaces (asphalt).
- Knee injury. This may include damage to the meniscus, displacement or fracture of the joint. This cause contributes to the development of the disease in young people. After fixation of the limb, blood circulation deteriorates. Damage to or removal of the meniscus leads to arthrosis in 90% of cases.
- Too much weight. Excessive weight can damage the meniscus. Restoration of the knee joint is protracted and difficult. In obese people, bilateral osteoarthritis of the knee is common. Another negative point is the presence of varicose veins. In this case, the patient develops the most severe form of knee gonarthrosis.
- Weakness of tape equipment. This causes too much joint mobility. Despite the fact that a person can sit on the twine without any problems even without warming up, at this time the joint gets microtrauma. If the knee is damaged enough, arthrosis begins to develop.
- Violation of metabolic processes. In this case, the knee joint does not receive enough nutrients.
- Joint pathologies. The pathology shown may be triggered by arthritis of the knee joint (reactive, rheumatoid). It is characterized by the development of inflammation and the accumulation of too much fluid in the joint cavity. The cartilage tissue in the knee begins to deteriorate.
- Stressful situation. Mood swings, the constant presence of the nervous system in a state of tension can provoke arthrosis of the knee joint.
- Congenital diseases of muscles, ligaments and dysplasia.
- Chondrocalcinosis (premature deposition of calcium salts in the cartilage of the knee). The pathology is systemic.
- Osteomyelitis. It is an inflammation of the bone marrow in which purulent masses are formed. They negatively affect the surrounding tissues. Over time, the purulent masses extend beyond the bone of the knee joint. Lack of treatment jeopardizes the development of sepsis.
- Acromegaly. It is an endocrine disease in which the levels of growth hormone - growth hormone - rise. Most often, benign tumors of the pituitary gland contribute to an increase in its volume. If such a disease develops in adolescence, the child has a specific physique. Excessive growth rate of cartilage tissue leads to deformation of the knee joint.
- Diabetes.
- Thyroid dysfunction. This disease is also endocrine. It occurs due to a lack of thyroid hormones. Man’s weight increases, he moves little, and the cartilage of the knee joint wears out.
- Freezing. In this case, ice crystals are formed in the soft tissues, which kill the living cells.
- Synovitis (inflammation localized in the synovial sac of the joint).
All of these causes can provoke knee gonarthrosis without even noticing when the disease began to develop.
What stages does arthrosis go through in its development?
The effectiveness of knee treatment depends on the degree of arthrosis diagnosed in the patient:
- The first stage of knee arthrosis. The pain is not very noticeable at this stage. The patient can endure the discomfort for years while not in a hurry to contact professionals or perform any treatment. A person needs help with an exacerbation. The sharp onset of pain is not characteristic of knee arthrosis.
- Grade 2 knee arthritis. The intensity of the discomfort increases. The pain occurs not only after physical exertion of the knee joint, but also at rest. To get rid of unpleasant feelings, you need to relax more. Swelling appears in the area of the knee joint, the patient hears a crack. The X-ray shows a narrowing of the joint space and a slight deformation of the knee joint.
- Grade 3 knee arthrosis. In this case, the mobility of the knee is severely limited and sometimes the foot cannot fully straighten. Joint pain becomes strong and permanent, appearing as a response to changing weather conditions. The discomfort is painful and difficult to get rid of even at rest. Often the patient’s sleep is disturbed and he uses NSAIDs to at least alleviate his condition. A person develops lameness and joint deformity is very noticeable.
Treatment for arthrosis should be started as early as possible before bone tissue destruction becomes critical. In the case of irreversible changes, only surgery will help the patient.
Symptoms of knee arthrosis
The development of arthrosis does not occur overnight. As it progresses, the symptoms become more intense. The following manifestations are characteristic of gonarthrosis:
- A crackle and click can be heard with a certain movement. The patient may notice this symptom quite late. However, he says the joint surfaces are damaged, with furrows and bone growths appearing on them.
- Swelling and enlargement of the knee.
- Painful feelings. They are invisible in the first stages of arthrosis and can only occur after a severe static load on the knee joint. Dynamic exercise, in turn, improves joint condition, nutrition, and subsequent prognosis. As the upper layer of cartilage is cleared in arthritis, the nerve endings are exposed. After a while (after rest), the fibers are covered with a small layer of fibrin and become less sensitive - the knee pain goes away. If the knee joint continues to collapse, the discomfort will not even leave the person alone. Edema appears in the bursa, which compresses the nerves even more. The inflammatory process begins.
- Limited mobility. This symptom allows arthrosis to be distinguished from other pathologies of the knee joint. Stiffness appears after sleep in the morning and disappears after half an hour. If this condition lasts for a long time, it indicates the presence of an inflammatory process.
- Reduced range of motion. The patient is unable to straighten the limb to the end. As the patient constantly feels pain, he tries to reduce the range of motion and the ligaments adapt to it. That is, they shorten and do not allow the knee joint to fully perform its function.
- Joint obstruction. It occurs as a result of strong changes in joint surfaces.
- Dislocations and subluxations. They appear in the last stage of arthrosis, when the joint is severely deformed.
Over time, one experiences muscle atrophy, proliferation of osteophytes, and weakening of the lateral ligaments. The consequences of arthrosis are severe as a person becomes disabled.
How is arthrosis defined correctly?
The patient should be thoroughly examined to begin the correct treatment of arthrosis. The diagnosis should be differentiated and include the following studies:
- X-ray of the knee joint. Gonarthrosis is performed in two projections. The specialist needs an x-ray of both the injured and the healthy knee. Radiography allows the identification of the following signs of arthrosis: joint space narrowing, osteophytes, subchondral sclerosis. In addition, the presented examination of the knee joint reveals the subluxation and ossification sites of the cartilage tissue.
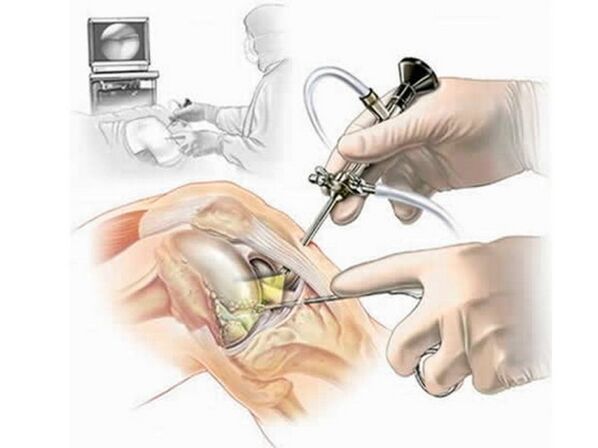
- Arthroscopy. It is a minimally invasive procedure used not only to diagnose but also to treat arthrosis. This requires the use of a special LED driver with a camera at the end. Insert through the small opening on the side of the knee. A complete picture of the internal state of the joint is reflected on the monitor. However, the method has one drawback: the joint is depressurized and pathogenic microorganisms can enter.
- Ultrasound. This diagnostic method is completely safe. The procedure helps to examine the soft tissues of the knee, as well as cartilage, joints, blood vessels.
- CT. This is an X-ray examination method, however, it allows you to see not only the bone structures but also the soft tissues. Thanks to the computer equipment, the specialist can create a three-dimensional model of the knee. However, in order to obtain accurate information, the patient must receive a significant dose of radiation.
- Scintigraphy. This is an X-ray using a contrast agent.
- MRI. In this case, magnetic rays are used to obtain the information. The image shows the soft tissues more clearly.
- Thermography. The procedure is based on the registration of heat radiation from the surface of the patient's body. So you can identify tumors, foci of inflammation. A test is assigned for differential diagnosis.
- General blood test. It helps to determine the severity of the inflammation, its nature.
- General urine test. Thanks to him, the systemic nature of the pathology can be determined.
- Blood chemistry.

Thanks to these diagnostic measures, professionals can accurately determine knee arthrosis and prescribe truly effective treatment.
Treatment of knee arthrosis
Treatment for arthrosis must be versatile and long-term. Because joint destruction cannot be completely stopped, therapy should be performed continuously to improve the patient’s quality of life.
Medications for the treatment of arthrosis
Your doctor may prescribe the following medications:
- Non-hormonal anti-inflammatory drugs. They are used in the form of tablets and ointments. However, in the case of severe pain syndrome that cannot be eliminated by standard methods, injection is used. It helps relieve pain quickly, relieve swelling and reduce the intensity of inflammation. These therapies can only eliminate the symptom, but they cannot cure arthrosis. Only a doctor can prescribe these funds. The course of treatment lasts for up to 14 days, and relief occurs in as little as 2-3 days.
- Chondroprotectors for knee arthrosis. All such drugs contain beneficial substances that are able to regenerate cartilage. However, this will only be effective if its application is launched on time. If the cartilage is completely wiped out, the use of chondroprotectors will be useless. Treatment with such devices will be long-term (at least 6 months). Tablets and topical medications are most commonly used, although injections are also possible.
- Vasodilators. They help relieve cramps and pain syndrome, restore normal blood circulation, and improve nutrition at the knee joint.
- Glucocorticosteroids. It is most often used in the most severe cases when other drugs do not give a positive effect. In arthrosis, intraarticular injections into the knee are used. They can only be used once a year.
- Enzymes. They ensure the regeneration of cartilage structure in the initial stages of the development of knee arthrosis. It is also prescribed to be injected into the joint.
- Hyaluronic acid. It provides smooth movement of the knee joint as it can replace the joint fluid.
- Topical preparations - ointments, creams, gels. They also only relieve the symptoms.
- Medicinal compression. In this case, a drug is used that can penetrate the skin, help eliminate muscle clamps, and have an absorbent effect. Compresses can be done with the help of medical bile.
Drug therapy is essential in the treatment of arthrosis. However, medications should be used strictly at the dose prescribed by your doctor. It is impossible to increase or decrease the rate on your own, to change the daily fee without the knowledge of a specialist.
Characteristics of physiotherapy treatment and exercise
Knee arthrosis can also be treated with physiotherapy procedures:
- Massage. It helps restore normal blood circulation to the tissues, eliminating muscle cramps.
- Drug electrophoresis makes it possible to eliminate inflammation in the joint and also results in an analgesic effect.
- Magnetic therapy. They stimulate the tissues surrounding the affected right or left joint using specific radiation. They improve cell metabolism.
- UHF. The waves promote the production of synovial fluid that lubricates the knee.
- Phonophoresis with corticosteroids.
- Electrotherapy eliminates not only pain but also swelling.
- Mud therapy.
- Hirudotherapy.
- Shockwave therapy.
- Heat treatment. This includes paraffin therapy. This procedure improves local blood circulation.
- SMV therapy. This physiotherapy stimulates blood circulation, relieves swelling and improves the nutrition of cartilage tissue.

Physiotherapy is extremely helpful. The flexibility of muscle tissue and ligaments needs to be restored, and the mobility of the knee joint needs to be improved. The following exercises will be helpful:
- Lying on your stomach, you should take turns raising your legs. In this case, do not bend at the knee. The lifting height is about 20 cm.
- Lying on your left, you should bend your left leg and raise it 30 degrees. In this position, the limb should be held for 30 seconds. The same exercise should be done with the right foot.
- When sitting on a chair, the legs should be straightened and lifted as high as possible one after the other.
The series of exercises is selected individually by the attending physician. Gymnastics is best if there are medicated ointments after a little massage. Physiotherapy is an effective adjunct to the treatment of arthrosis that enhances the effects of medications.
Do you need surgery?
In the most severe cases, when the joint is severely destroyed due to arthrosis, the patient is prescribed surgery. There are several types of interventions:
- Articulated traction. This includes stretching the joint damaged by arthrosis to increase the gap between the cartilages. This makes it possible to prevent further tissue destruction and gradual recovery.
- Endoprosthetics is the complete replacement of a joint destroyed by arthrosis. They are implemented as a last resort. The replacement may be complete or partial. The prosthesis must be replaced after 10-15 years.
- Osteotomy. Such treatment of arthrosis allows for the mechanical correction of abnormalities in severely deformed bones. In this case, the solid elements break at a strictly defined location. The bones are then correctly positioned and fused.
- Arthroscopy. It is used to restore the surface of cartilage destroyed by arthrosis. In addition, an arthroscope can be used to remove foreign bodies and bone fragments from the joint. Such an operation is used for joint hypermobility. Arthroscopy is considered a low-traumatic procedure, so rehabilitation afterwards does not take long.
It is better not to bring it to surgery. Treatment should be started in the first stage of arthrosis. Orthopedic devices help to consolidate the result: reeds, orthosis to reduce the load, knee braces with infrared radiation.
Use of folk remedies
Complete cure of arthrosis is impossible as the degenerative process progresses gradually. However, it can eliminate the symptoms and stop the destruction of the knee joint in arthrosis. Folk remedies can be used during aggravation as well as during periods of relative calm. But first you need professional consultation. The following recipes may be helpful for arthrosis:
- The roots of chopped horseradish should be boiled in a small amount of water at low temperature. The bag should then be filtered and placed around the knee affected by arthrosis. The compress should be fastened with a bandage. You must complete the procedure every day for a month. Compresses improve blood circulation and tissue repair.
- If you rub any vegetable oil into the area of the knee joint due to arthrosis, the pain will go away. However, it needs to warm up a bit.
- The mummy makes a good impression. It is necessary to mix 3-4 g of raw material with 100 g of honey and mix everything thoroughly. In the evening, before going to bed, you should rub the medicine on the sore spot. Then wrap the affected area with a warm scarf. The reception of the mummy inside is also welcomed. You can use it with a daily dose of 0. 2 g.
- Fresh dandelion flowers can be washed thoroughly and consumed 5-6 pieces per day. Dry ingredients can be in 1 tablespoon. pour a glass of boiling water, stick to it and drink 1/3 cup three times a day.
- Rubbing aloe leaves. It is necessary to twist the 10 sheets of the plant and press it through the cheesecloth. The juice is mixed with half a glass of honey and 150 ml of red wine. The resulting product was poured into a dark glass container and applied daily for one month.
The leaves of cabbage and burdock help relieve the inflammation of arthritis. Folk remedies are not considered a panacea, but they increase the effectiveness of other therapies.
Dietary rules for arthrosis
Treating arthrosis does not require a particularly strict diet, but you still need to follow certain dietary rules:
- Reduce salt intake. Its total daily amount should not exceed 2 g. It is better to salt the pan immediately before use and not while cooking.
- The amount of spices used in the treatment of arthrosis should also be reduced. The same applies to fermented foods and pickles. Marinades and preserves are usually better excluded from the diet.
- Animal fats are not recommended.
- The menu should not include sweets, cakes and bread made from wheat flour.
- In arthrosis, alcohol and nicotine are strictly prohibited.
- Foods containing gelatin are useful: aspic, jelly meat, beef bone soups.
- Consumption of milk protein (products should not be fatty), fish, seafood is important for arthrosis.
- The diet should include vegetable oils, vegetables and fruits, freshly squeezed juices.
- A person should consume a sufficient amount of fluids daily.

The proper diet for arthrosis should be developed by a professional. You can’t overdo it even if the patient is overweight. Dramatic and improper weight loss only worsens your health. In this case, treatment is significantly delayed.
Prevention of arthrosis
To avoid the development of osteoarthritis and to lose your ability to walk, you should follow the following expert advice:
- We must not forget about movement. We better go to the pool, ride a bike, hike in the fresh air. You can also dance.
- It is advisable to avoid possible lesions and hypothermia of the knee joint, as this provokes post-traumatic arthrosis.
- For prolonged loading, it is better to use a protective knee pad or other orthopedic device.
- It is advisable to wear comfortable shoes.
- Proper eating is important - there is no chance of arthrosis if all the necessary nutrients are regularly supplied to the joint.
- If you are overweight, get rid of it.
- It is better to avoid stress and to organize your work and rest routine properly.
- The body's defenses need to be strengthened.
- Any inflammatory or infectious pathology that may trigger the development of arthrosis should be eliminated in a timely manner.

Proper prevention can significantly delay the destruction of joints, which is normally the body’s natural aging process.
Arthrosis of the knee joint is an incurable disease, but its progress can be slowed down or even stopped by improving the quality of life.

























